Platelet-Rich Plasma (PRP) therapy has emerged as a promising regenerative treatment in various medical fields, including reproductive medicine. This article delves into the application of Platelet-Rich Plasma therapy for infertility, focusing on uterine and ovarian rejuvenation, and reviews recent scientific research and case studies highlighting its effectiveness.
What is Platelet-Rich Plasma Therapy?
PRP therapy involves the extraction and concentration of platelets from a patient’s own blood. These platelets are rich in growth factors and cytokines, which play a crucial role in tissue repair and regeneration. The process includes drawing blood, centrifuging it to separate the components, and injecting the concentrated platelets into the targeted tissue to promote healing and rejuvenation.
Why is PRP Used for Treating Infertility?
In reproductive medicine, PRP therapy is utilized to enhance the function of reproductive organs. Its regenerative properties are believed to improve the microenvironment of the ovaries and uterus, potentially leading to better fertility outcomes. PRP is considered for patients with conditions such as poor ovarian reserve, thin endometrial lining, or those experiencing recurrent implantation failure.
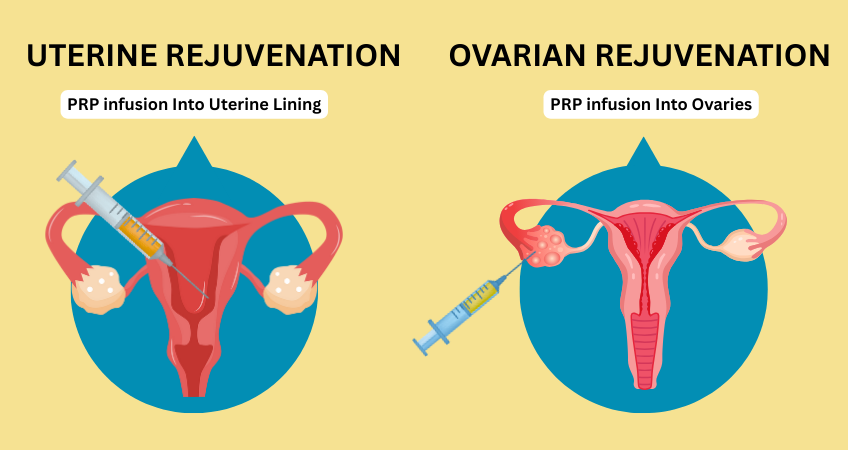
Uterine Rejuvenation with PRP Therapy
A receptive endometrium is vital for embryo implantation. Some women suffer from thin endometrial lining, which can hinder successful implantation and pregnancy. Intrauterine infusion of PRP has been explored as a method to enhance endometrial thickness and improve implantation rates.
Scientific Research on PRP for Uterine Rejuvenation
Platelet-Rich Plasma: A Promising Regenerative Therapy in Gynecological Disorders: A study published in the Journal of Ovarian Research reviewed the effectiveness of PRP in endometrial abnormalities. The findings suggested that PRP infusion could restore endometrial structure and decrease fibrosis, thereby improving pregnancy outcomes in conditions like Asherman’s syndrome.
Ovarian Rejuvenation with PRP Therapy
Ovarian aging and diminished ovarian reserve are significant challenges in fertility treatments. PRP therapy aims to rejuvenate ovarian tissue, potentially restoring hormonal balance and enhancing oocyte production.
Scientific Research on PRP for Ovarian Rejuvenation
Platelet-rich plasma (PRP) treatment of the ovaries significantly improves fertility parameters and reproductive outcomes in diminished ovarian reserve patients: a systematic review and meta-analysis: A systematic review and meta-analysis published in the Journal of Ovarian Research analyzed the impact of intraovarian PRP administration on patients with diminished ovarian reserve. The study concluded that PRP treatment significantly improved fertility parameters and reproductive outcomes in these patients.
Case Studies Highlighting PRP Therapy Effectiveness
Uterine Rejuvenation Case Study
A case series reported in the Journal of Clinical Medicine detailed the treatment of a woman in premature menopause using autologous PRP. The patient experienced restored menstrual cycles and achieved a successful pregnancy following PRP therapy:
Autologous Platelet-Rich Plasma Treatment Enables Pregnancy for a Woman in Premature Menopause Authors: Konstantinos Sfakianoudis, Mara Simopoulou, Nikolaos Nitsos, et al. Published in: Journal of Clinical Medicine, December 2018 – PubMed
Summary:
This case study details the treatment of a 40-year-old woman who had been experiencing premature menopause since the age of 35. The patient declined oocyte donation and opted for an innovative approach involving the intraovarian injection of autologous PRP to rejuvenate ovarian tissue and facilitate the use of her gametes through in-vitro fertilization (IVF). Six weeks following the PRP treatment, a significant reduction in follicle-stimulating hormone (FSH) levels was observed, indicating improved ovarian function. Subsequently, a natural IVF cycle was initiated, leading to a biochemical pregnancy. Unfortunately, this resulted in a spontaneous abortion at the fifth week of gestation. Despite the miscarriage, this case represents the first reported instance of autologous PRP application leading to pregnancy in a menopausal patient, suggesting a potential avenue for fertility restoration in similar cases.
Ovarian Rejuvenation Case Study
A pilot study involving 253 women assessed the efficacy of intraovarian PRP infusion. The results indicated that the majority of participants showed improved hormonal profiles, and 17% successfully conceived post-treatment. Read on:
A Case Series on Natural Conceptions Resulting in Ongoing Pregnancies in Menopausal and Prematurely Menopausal Women Following Platelet-Rich Plasma Treatment.
Authors: Konstantinos Pantos, Mara Simopoulou, Agni Pantou, et al. Published in: Cell Transplantation, July 2019 . Sage Journals
Summary:
This case series reports on three women—aged 40, 27, and 46—diagnosed with premature ovarian failure (POF) or menopause, each experiencing amenorrhea for over a year and having a history of unsuccessful IVF attempts. Rejecting oocyte donation, they elected to undergo autologous ovarian PRP treatment. Post-treatment, all three patients experienced the restoration of their menstrual cycles and demonstrated improved hormonal profiles, including decreased FSH levels and increased anti-Müllerian hormone (AMH) levels. Remarkably, within 2 to 6 months following PRP therapy, each woman conceived naturally, leading to ongoing, complication-free clinical pregnancies at the time of reporting. This series is the first to document natural conceptions and ongoing pregnancies in menopausal and prematurely menopausal women following PRP treatment, highlighting the potential of this therapy in restoring ovarian function and fertility.
These case studies underscore the emerging role of PRP therapy in reproductive medicine, particularly for women with diminished ovarian reserve or premature menopause. While the outcomes are promising, further extensive research is necessary to establish standardized protocols and confirm the efficacy and safety of PRP treatments in such contexts.
Conclusion
Platelet-Rich Plasma Therapy for treating Infertility presents a novel approach in the realm of ART, offering hope to individuals facing challenges related to uterine and ovarian function. While preliminary studies and case reports are promising, further large-scale, randomized controlled trials are necessary to establish standardized protocols and confirm the efficacy and safety of PRP therapy in reproductive medicine.
Note: This article is for informational purposes only and does not constitute medical advice. Individuals should consult with healthcare professionals for personalized recommendations.
For personalized advice and to explore if PRP therapy is right for you, consult with a fertility specialist.