IUI Treatment Process, Important considerations, Success Rates, and Cost Explained
Intrauterine insemination (IUI) is a baseline treatment advised for couples facing infertility challenges. It offers a simple and effective method to increase the chances of successful fertilization and pregnancy. But is IUI is always the right treatment for all couples? Consulting with a fertility specialist is crucial to determine if IUI is the right choice for you, based on individual circumstances and discussion of the potential benefits in achieving pregnancy. In this article we will provide all the information you need about IUI treatment process, cost and success rates and important considerations
How Does IUI Help?
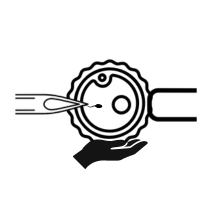
IUI, involves placing specially washed and prepared sperm directly into the uterus, bypassing the cervix. This procedure is timed to coincide with a woman’s ovulation, maximizing the chances of fertilization and pregnancy. The rationale behind the treatment is by providing a controlled environment for sperm placement and timed ovulation, IUI addresses various fertility factors, such as mild male factor infertility, cervical issues, or irregular ovulation and improves the chances of fertilization.
When is it recommended?
It is a preferred treatment for coupes with Male Factor Infertility. In other words, Doctors consider IUI as a first-line treatment, if the male partner has problems like Sexual dysfunction, premature ejaculation, Abnormalities in Penile curvature etc or in cases of mild male factor infertility (like decreased sperm count or motility), in such cases an IUI procedure is recommended. The success rate of treatment with IUI is high if this is the couple’s primary infertility issue.
IUI may also be recommended in the following situations:
- Unexplained Infertility: When no clear cause for infertility has been identified, IUI can be an initial treatment option.
- Mild Male Factor Infertility: If the male partner has a low sperm count, decreased motility, or mild sperm abnormalities, IUI can help facilitate the sperm’s journey to the fallopian tubes, increasing the chances of fertilization.
- Cervical Factor Infertility: In cases where the cervix poses a barrier to sperm entry or if the cervical mucus quality is suboptimal, IUI can help bypass these challenges.
- Ovulation Disorders: Women with irregular or absent ovulation patterns may benefit from IUI when combined with ovulation induction medications. These medications stimulate the growth and release of mature eggs, improving the chances of successful fertilization.
- Endometriosis-Related Infertility: IUI can be considered for couples where endometriosis is present but not severely affecting fertility.
To Know more read : Who Should Consider IUI for Infertility?
When is IUI treatment not considered?
While IUI is helpful for a number of patients experiencing infertility that hope to conceive, there are certain situations in which it’s not an ideal treatment option. This includes the following cases:
- Severe male factor infertility
- Females with both fallopian tubes blocked
- or Disease affecting the fallopian tubes
- Medical history of pelvic adhesions
- Females with severe pelvic infection
- Males with less than 1 million sperm count in post semen wash
- Severe endometriosis
IUI is not an option if Male partner is suffering from ejaculatory disorders like anejaculation or retrograde ejaculation or severe male factor infertility in which case, we can’t obtain a sample for IUI.
In addition, people who have had not achieved success with IUI after multiple IUI attempts in the past will have other fertility treatments recommended to them. IUI isn’t usually recommended for intended mothers over 40.
Learn what are the Best Practices for IUI success rates that Clinics practice.