Planned Coitus with Follicular Monitoring (PCM): A Natural Approach to Boost Fertility
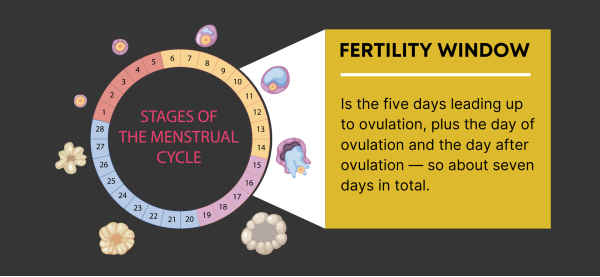
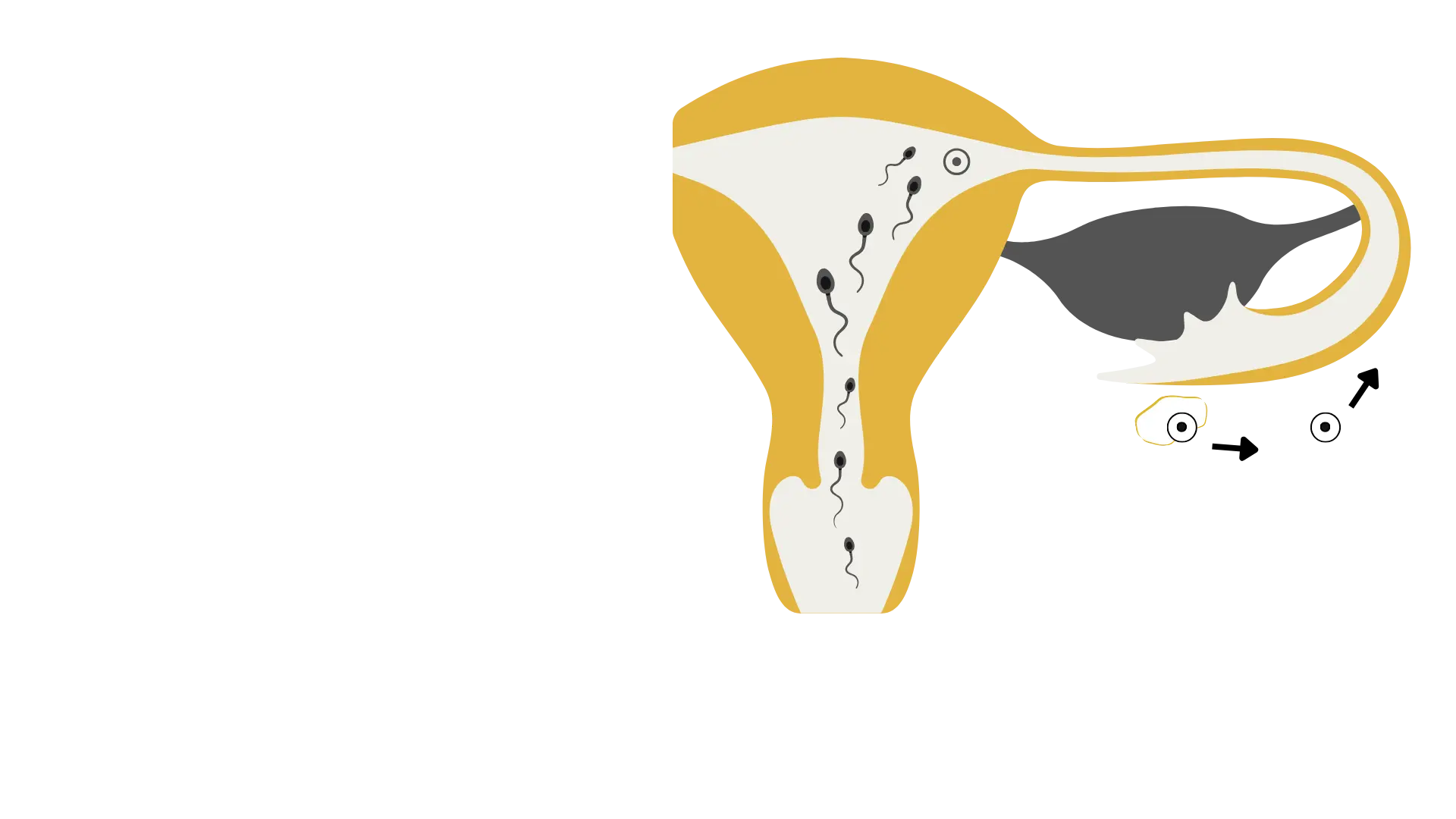
Planned Coitus with Follicular Monitoring, also known as Timed Intercourse (TI) is one of the low-intervention – basic fertility treatment options recommended to couples who are unable to conceive naturally. PCM or TI is a natural, non-invasive fertility approach that helps couples optimize their chances of conception by accurately tracking ovulation. Simply put, it helps in scheduling Intercourse around your “fertile window”. This method involves using ultrasound scans to monitor follicular development in the ovaries, ensuring that intercourse is timed precisely when ovulation is about to occur. By identifying the most fertile days, this approach maximizes the likelihood of sperm meeting the egg, leading to successful fertilization.
Follicular monitoring is typically performed between days 9 to 16 of the menstrual cycle, depending on cycle length. It involves a series of transvaginal ultrasounds to assess follicle growth, endometrial thickness, and the exact timing of ovulation. Once a mature follicle is detected, couples are advised to have intercourse within 24 to 36 hours, which is the optimal window for conception.
This method is especially beneficial for couples facing irregular ovulation, unexplained infertility, or mild hormonal imbalances. It is also useful for those trying to conceive naturally before considering assisted reproductive techniques like intrauterine insemination (IUI) or in vitro fertilization (IVF). Unlike fertility treatments that involve medications or invasive procedures, planned coitus with follicular monitoring works in harmony with the body’s natural cycle, making it a preferred option for many couples.
Scientific studies have shown that timed intercourse with follicular tracking improves pregnancy success rates, particularly in couples who have been trying to conceive for over six months. It reduces guesswork and provides a scientific basis for determining the most fertile period in a woman’s cycle.
By combining advanced ultrasound technology with a natural conception strategy, planned coitus with follicular monitoring empowers couples with the knowledge they need to enhance fertility, reduce stress, and increase their chances of achieving a healthy pregnancy.
For personalized advice and to explore if PCM is right for you , consult with a fertility specialist.