What is HLA Compatibility
HLA compatibility refers to how similar two individuals’ human leukocyte antigens (HLAs) are. HLAs are proteins found on the surface of most cells in your body, and they play a key role in how the immune system recognizes what belongs in the body and what doesn’t. HLA compatibility between two individuals can be measured by doing a simple Lab test call HLA typing.
What is HLA typing?
HLA typing (Human Leukocyte Antigen typing) is a lab test used to identify a person’s specific HLA genes. These genes are part of the major histocompatibility complex (MHC) and are crucial for immune system functioning—especially for distinguishing self from non-self.
What does it Measure?
It identifies which versions (alleles) of HLA genes a person has, particularly from these groups:
- Class I HLAs: HLA-A, HLA-B, HLA-C – found on nearly all cells
- Class II HLAs: HLA-DR, HLA-DQ, HLA-DP – mostly found on immune cells
Why is HLA typing Done?
- Organ and Stem Cell Transplants: Matching HLA types between donor and recipient reduces the risk of transplant rejection.
- Disease Association: Certain autoimmune conditions (like Type 1 diabetes, celiac disease, lupus) are linked to specific HLA types.
- Reproductive Medicine: In some fertility clinics, HLA typing is used to explore causes for:
- Recurrent miscarriages
- Repeated IVF failures
- Potential maternal-fetal immune compatibility issues
- Paternity Testing or Genetic Ancestry: Occasionally used in forensic or genealogical contexts.
Understanding HLA compatibility in context of Pregnancy
In the context of pregnancy, HLA compatibility refers to the matching of Human Leukocyte Antigens between a mother and fetus. HLA compatibility can impact pregnancy success by influencing the mother’s immune response towards the fetus, with some studies suggesting that a moderate level of HLA mismatch might be beneficial for a successful pregnancy, while too much matching (high compatibility) could potentially increase the risk of pregnancy complications like recurrent miscarriages or preeclampsia. Essentially, a delicate balance is needed for the immune system to tolerate the fetus without aggressively attacking it.
Key points about HLA compatibility and Pregnancy:
HLA compatibility can influence pregnancy outcomes in the following ways:
- Immune Tolerance:
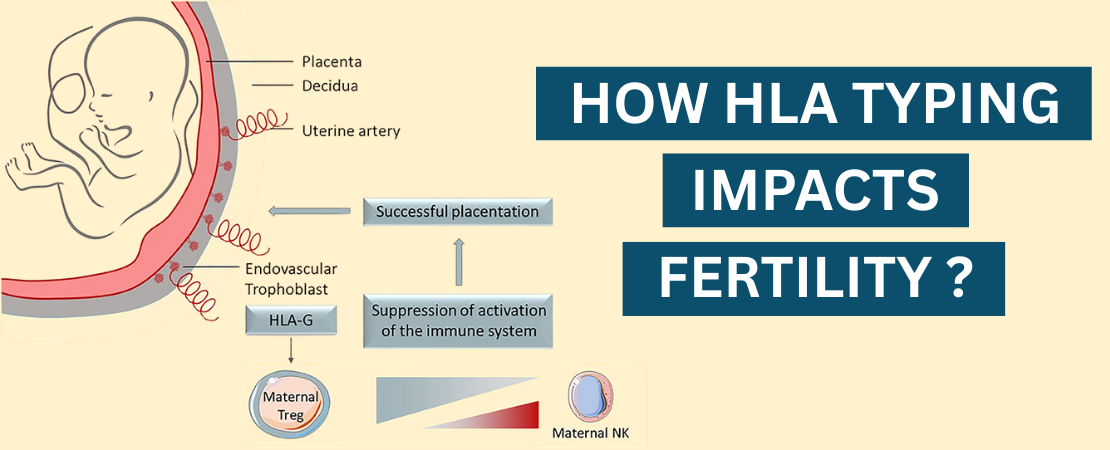
- During pregnancy, the mother’s immune system must tolerate the fetus, which contains genetic material from the father (including his HLAs). The placenta expresses a specific HLA molecule called HLA-G, which helps suppress the mother’s immune system and prevent rejection of the fetus.
- Some research indicates that a moderate level of HLA mismatch between mother and fetus can trigger the development of regulatory immune cells, which are crucial for maintaining pregnancy tolerance.
- If the fetus’s HLA molecules are too similar (i.e., highly compatible) to the mother’s, her immune system might not properly recognize the fetus as “foreign” enough to trigger the necessary immune adaptations for pregnancy support.
- Natural Killer (NK) Cells and HLA:
- The interaction between maternal uterine NK cells and fetal HLA-C molecules is critical. Poor interaction due to too much or too little HLA compatibility can disrupt implantation or placental development.
HLA Dissimilarity between Partners is Often Beneficial for Pregnancy:
- Some studies suggest that a certain level of HLA mismatch between partners can be beneficial, promoting better immune tolerance mechanisms (like more effective regulatory T cells).
- This helps reduce the risk of pregnancy complications such as recurrent miscarriage, preeclampsia, and implantation failure in IVF.
Potential risks with high HLA compatibility between partners:
High HLA compatibility between partners—meaning their immune systems are very similar—can pose some unique reproductive risks, especially from an immunological standpoint. Here’s how:
- Reduced Immune Activation: The maternal immune system might not recognize the embryo as sufficiently “foreign.” This is important because a certain level of immune activation is crucial for proper implantation and placental development. Without that signal, the body may not provide the necessary immune tolerance mechanisms, like regulatory T cells, to protect the pregnancy.
- Increased Risk of Recurrent Miscarriage: Studies suggest a link between high HLA compatibility and recurrent pregnancy loss (RPL). The theory is that the embryo is not triggering a strong enough maternal immune response, leading to inadequate support for fetal development.
- Implantation Failure in IVF: In assisted reproductive technologies, embryos from highly HLA-compatible couples may fail to implant due to lack of immune modulation needed for successful implantation.
- Impaired Natural Killer (NK) Cell Interaction: Uterine NK cells interact with fetal HLA-C molecules to promote proper placental development. High HLA similarity can disrupt this communication, potentially leading to:
- Poor placental formation
- Preeclampsia
- Fetal growth restriction
Autoimmune-Like Response: In some cases, high compatibility may confuse the immune system, failing to mount proper tolerance or even reacting against the pregnancy as if it were abnormal tissue.
Note:
While these risks are supported by some clinical observations and immunology research, the evidence isn’t universal, and not all fertility specialists test for HLA compatibility. It’s often only explored in cases of recurrent IVF failure or unexplained miscarriages.
To know more about Immune Factors and how they affect fertility read: Immune Related Fertility Challenges
Additional Reading :
Human Leukocyte Antigen Alleles Compatibility and Immunophenotypic Profile Associations in
Infertile Couples: This study investigates the association between HLA-DQA15 allele compatibility in couples and reproductive outcomes. It found that couples in which both partners carry the HLA-DQA15 allele have a higher likelihood of increased HLA-DQA1 compatibility. This heightened compatibility was associated with recurrent miscarriages and IVF failures, suggesting that HLA-DQA1*5 could serve as a marker for assessing immunological compatibility in infertile couples.
Primary Infertile Couples Share More HLA Alleles Than Expected by Chance: A Case–Control Study: This recent study examines the HLA allele sharing among primary infertile couples compared to fertile controls. The findings indicate that infertile couples share a significantly higher number of HLA alleles than would be expected by chance. This suggests that HLA similarity between partners may contribute to infertility, highlighting the potential importance of HLA typing in infertility diagnostics and treatment planning.
Immunogenetic determinants in recurrent miscarriage – evidence from genetic-epidemiological research: In his 2002 study titled “Immunogenetic Determinants in Recurrent Miscarriage – Evidence from Genetic-Epidemiological Research,” Dr. Ole B. Christiansen explores the immunogenetic factors contributing to recurrent miscarriage (RM). He examines how maternal immune responses, particularly those involving human leukocyte antigen (HLA) compatibility and natural killer (NK) cells, may influence pregnancy outcomes. The study suggests that certain HLA class II alleles, such as DR1 and DR3, might predispose women to RM by promoting a Th1-type immune response, which is detrimental to fetal tolerance. Additionally, the research indicates that abnormal interactions between uterine NK cells and trophoblast HLA molecules could impair placental development, further contributing to pregnancy loss. Christiansen’s work underscores the complexity of immunogenetic interactions in pregnancy and highlights the need for further research to develop targeted interventions for women experiencing RM.